The challenge to identify and address health disparities tied to social vulnerabilities is by no means a new problem. It’s well known that marginalized communities face barriers to healthcare access, leading to disparate outcomes in patient care and population health management. Health equity has recently been thrown into even sharper focus, with the COVID-19 pandemic highlighting the depth and severity of these disparities in infection rates, mortalities, and therapeutic access.
Research tells us that health inequities account for approximately $320 billion in annual United States healthcare spend and could reach $1 trillion by 2040 if left unaddressed. Furthermore, social determinants of health (SDoH) are among the most significant health status predictors and may contribute up to 90% of health outcomes variability. Despite that, less than 25% of today’s hospital care or screening models consider social needs.
Equity-focused approaches should recognize and incorporate how SDoH factors (poverty, social/racial/ethnic discrimination, and housing/transportation conditions) contribute to health and disease status. Multiple stakeholders can use those insights to ensure that health services and therapeutics are accessible, affordable, and culturally competent or appropriate for diverse populations.
An Easy Problem to Diagnose, A Hard One to Solve
A crucial blocker here is the data, both its scarcity and its quality, and thus where and how to implement and assess effective interventions. Studies tasked with understanding disparate health outcomes and determining value-based market access and pricing — or direct more inclusive trials in new therapeutic development — rely on data signals within patient claims and electronic health or medical (EHR or EMR) records. Yet these data sources are inherently biased. Service barriers can lead to the underrepresentation of marginalized groups when a disease (such as cancer or other chronic conditions) goes undetected or undiagnosed. Likewise, those groups can be overrepresented in late-stage or severe outcomes (like emergency hospitalizations) due to a lack of preventative care or early detection support.
Suppose we supplement this with all the varied sources of behavioral and social data (both at individual and community level), though. In that case, it can become dangerously like the Everything Bagel from Everything Everywhere All at Once!
How can we prioritize regional areas for a given disease and begin to understand more granularly how different social factors may contribute to health outcomes? How can we use those insights to direct our focus to the collection and utility of data to better address health equity?
Drive Health Insights With Community-Level Data
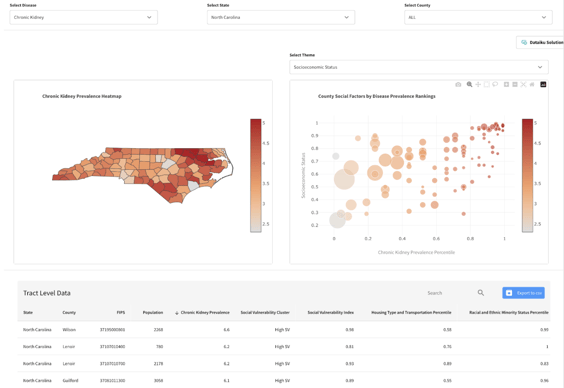
Dataiku’s SDoH solution focuses on leveraging local area data (U.S. Census and CDC surveys at the county and tract level) with goals to optimize regional health outreach, services, and therapeutic access programs by discovering community-level SDoH impacts on chronic disease prevalence patterns.
This plug-and-play solution helps to address challenges in understanding how social factor vulnerabilities underpin chronic disease prevalence to promote equity through:
- Drug and device manufacturers in effective market access, HCP engagement, risk surveillance, and inclusive clinical trial design to remove social factor bias
- Hospitals and health services organizations in practice and outreach programs tailored to social needs
- Health insurers in promotions and care coverages to reduce the burden on the U.S. healthcare system from preventable disease
Solution Key Features
The key deliverables of this solution encourage healthcare professionals to drive the inclusion of SDoH in market access, care, and coverage. A health equity web application lets users discover regions based on disease prevalence and social vulnerability themes. The web application can be deployed into external systems for health equity outreach.
Dataiku provides a reproducible, automated flow for pulling public data via API from the U.S. Census on social factor conditions, as well as data from the Center for Disease Control and Prevention on chronic disease prevalence and risk behaviors surveys. These complex data undergo preprocessing to convert the community social factor information and health-related outcomes to actionable analytic insights.
Interpretable regression models are trained to explore social factors’ impact on chronic disease prevalence. Users can go deeper via SHapley Additive exPlanations (SHAP) to find social vulnerability features important to community disease prediction. Regional segmentation can scale social programs and outreach efforts. We cluster communities based on social factor rankings to discover potential regional patterns in undiagnosed chronic diseases. Those insights align the cluster trends across diseases and may optimize program outreach nationally.
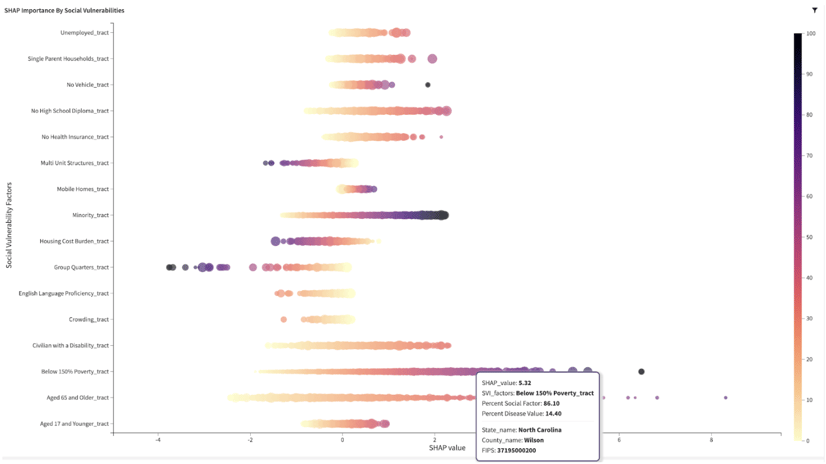
Lastly, Interactive visual dashboards allow drug manufacturers to incorporate social disparities in therapeutic market access. We further enable health systems to drive improved care programs tailored to social needs and insurers to build responsible coverage plans to increase disease treatment and outcomes equity.
Get Solving With Dataiku
This solution intends to enable healthcare and life science professionals to understand how Dataiku can be used to accelerate the discovery of how SDoH disparities affect at-risk populations. The immediate insights can be used to refine market access strategies for drug manufacturers, create new coverage policies from payers, and improve facility outreach and care programs from health services.
With a Responsible AI mindset, users should promote and prioritize health equity and therapeutic access instead of re-enforcing or deepening disparities or biases in the health and life sciences systems.




